1. Introduction
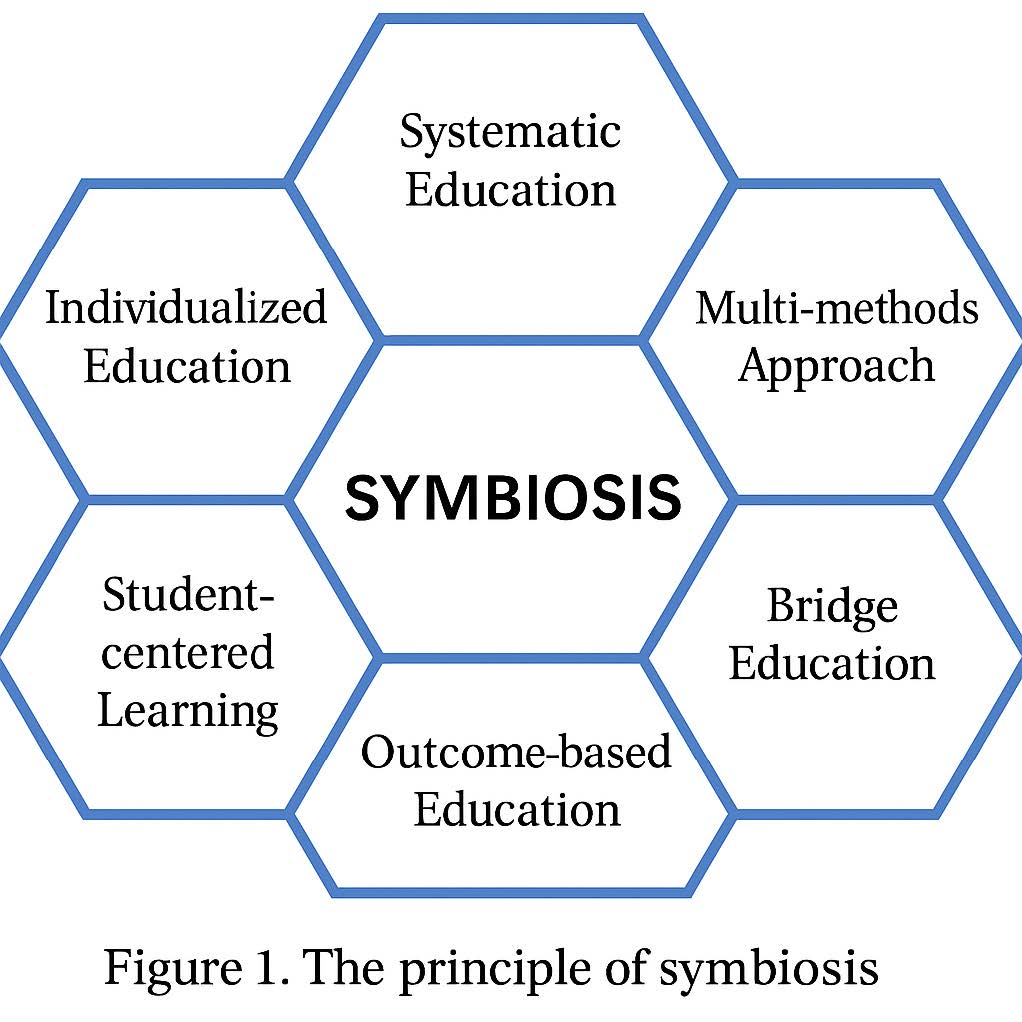
Pusan National University School of Medicine (PNUSOM), one of Korea's leading national medical schools, has cultivated a strong identity rooted in social responsibility, academic excellence, and innovation. With a proud history dating back to 1946, PNUCM has continually evolved to meet the needs of modern healthcare while maintaining its mission to train competent, compassionate, and future-oriented physicians. Central to our curriculum is the SyMBIOSIS framework, a uniquely structured educational philosophy that governs how we develop, deliver, and refine our medical education. Our curriculum is designed to prepare "Competent Pusan Medical Students" who will become outstanding physicians capable of meeting current and future healthcare challenges.
2. The SyMBIOSIS Educational Framework
Systematic Education
- Seamless Integration: Pre-medical to medical school transition with systematic competency management
- Comprehensive Competency Tracking: From admission to graduation, ensuring systematic development of student capabilities
- Vertical Alignment: Coordinated progression through all educational phases
Multi-methods Approach
- Diverse Teaching Methods:
- · Problem-Based Learning (PBL)
- · Collaborative learning
- · Internet-assisted learning
- · Standardized patient utilization
- · Role-playing and clinical skills training
- · Team-based learning
- · Early clinical exposure through shadowing programs
- · Peer-to-peer cooperative learning for CPX/OSCE preparation
- Comprehensive Assessment Methods:
- · Written examinations, practical assessments, and oral examinations
- · PBL evaluations, assignments, quizzes, and attendance tracking
- · Evidence-based medicine integration with PBL modules
Bridge Education (Enhanced Transition)
- Smooth Phase Transitions: Specialized courses for seamless academic progression
- · "Doctor and Leadership" for first-year pre-medical students
- · "Introduction to Clinical Medicine" for medical school entry
- · Pre-clinical training preparation
- · Post-graduation education consideration
- Comprehensive Transition Support:
- · Interview techniques and communication skills
- · Clinical skills integration
- · Professional development programs
- · Shadowing experiences
- · Student internship programs
Integration
- Horizontal Integration: Foundational medical sciences coordination
- Vertical Integration: Basic sciences, clinical medicine, and medical humanities
- Spiral Curriculum Design: Important concepts reinforced through meaningful repetition
- System-Based Integration (SBI): Disease pattern-based integrated education
Outcome-based Education
- Clear Learning Outcomes: Five core graduation competencies (CPM²S)
- Systematic Assessment: Phase-specific outcome evaluation
- Continuous Monitoring: Regular assessment of competency achievement
- Evidence-Based Progression: Advancement based on demonstrated competency
Student-centered Learning
- Active Learning Emphasis: Student participation in diverse educational activities
- Individualized Support: Formative assessments to enhance student learning
- Critical Thinking Development: Evidence-based learning approaches
- Self-directed Learning: Encouraging independent inquiry and research
Individualized Education
- Flexible Elective Courses: Tailored to individual interests and career goals
- Portfolio-Based Assessment: Personal development tracking
- Mentorship Programs: Faculty guidance for individual student development
- Research Opportunities: Individual and group research projects
Sustainable Education System
- Adaptive Curriculum: Responsive to changing social and healthcare needs
- Future-Oriented Training: Preparation for evolving medical practice
- Lifelong Learning Foundation: Skills for continuous professional development
- Social Responsibility: Addressing community health needs and social equity
3. Curriculum Structure: Three Phases of Medical Education
Phase 1: Pre-Medical Foundation (Years 1-2 Pre-med)
- Natural Sciences and Humanities: Comprehensive foundation building
- Research Methods: Early introduction to scientific inquiry
- Portfolio Development: Self-reflection and goal setting
- Service Learning: Community engagement and social responsibility
Phase 2: Integrated Medical Sciences (Pre-med Year 2 Semester 2 - Medical Year 2)
Foundation of Medicine (Horizontal Integration)
- Human Structure I & II
- Cell Regulation
- Human Metabolism
- Disease Understanding and Pharmacotherapy
System-Based Integration (SBI) - Vertical Integration
- Clinical Medicine Introduction
- Infectious Diseases
- Digestive System and Nutrition
- Cardiovascular System
- Respiratory System
- Endocrine System
- Renal and Urological System
- Hematology and Oncology
- Reproductive Medicine
- Growth, Development, and Aging
- Immunology and Dermatology
- Musculoskeletal System
- Psychiatry
- Neurology and Special Senses
Phase 3: Clinical Practice (Medical Years 3-4)
- Required Clinical Rotations (37 weeks): Core specialties including Internal Medicine, Surgery, Pediatrics, Obstetrics & Gynecology, Psychiatry, Family Medicine, Emergency Medicine
- Elective Clinical Rotations (12 weeks): Specialized departments and international experiences
- Student Internship (4 weeks): Deep clinical engagement as primary care providers
- Community Medicine Practice (1 week): Public health and community engagement
- Advanced Clinical Performance Course: Intensive preparation for national examinations
4. Distinctive Educational Features
Early Clinical Exposure
- Shadowing Programs: Beginning in medical year 1, students observe practicing physicians
- Progressive Clinical Skills: Stage-appropriate clinical skills training throughout the curriculum
- Patient Care Participation: Graduated responsibility in patient care
Evidence-Based Medicine Integration
- Research Skills Development: From pre-medical through clinical years
- Critical Literature Review: Integrated with PBL modules
- Clinical Decision Making: Evidence-based approaches to patient care
- Medical Research Program: Multi-year research projects with faculty mentorship
Medical Humanities Integration
- Comprehensive Coverage: Philosophy, history, culture, ethics, law
- Clinical Ethics: Patient safety, communication, and professionalism
- Social Medicine: Community health and healthcare systems
- Reflective Practice: Portfolio-based self-assessment and growth
International Perspectives
- Global Health Awareness: Future medicine and international healthcare trends
- Exchange Programs: Clinical rotations at partner institutions
- · Universities in USA (Hawaii), France (Lille), Japan (Kyushu, Nagasaki), Taiwan, Thailand, Indonesia, Uzbekistan
- Cultural Competency: Preparing graduates for global medical practice
Assessment and Quality Assurance
- Comprehensive Evaluation System: Multiple assessment methods aligned with learning outcomes
- Continuous Improvement: Regular curriculum review and enhancement
- Student Feedback Integration: Active student participation in curriculum development
- External Accreditation: Meeting international medical education standards
5. Graduation Competencies (CPM²S)
Our graduates achieve five core competencies:
- 1. Communication and Collaboration
- 2. Professionalism
- 3. Medical Competency (Medical Knowledge & Patient Care/Skills)
- 4. Scholarly Attitude (Lifelong Learning & Research)
Communication & Collaboration
| Sub-competency | Description | Behavioral Indicators |
|---|---|---|
| 1. Mechanisms of Health and Disease | Ability to explain the mechanisms underlying medical problems. | Explains the normal structure and function of the human body. Understands the pathophysiology of diseases and applies it to diagnosis and treatment. Describes the symptoms and progression of common diseases. |
| 2. Diagnostic Investigation | Ability to appropriately select and interpret diagnostic tests based on clinical presentations to identify and reason through clinical problems. | Selects appropriate diagnostic methods necessary for diagnosis and treatment. |
| 3. Therapeutic Approach | Ability to appropriately select, apply, and evaluate treatment methods in clinical situations. | Selects and applies evidence-based medical/surgical treatments for major clinical situations. Selects and applies appropriate medications for different diseases. |
Professionalism
| Sub-competency | Description | Behavioral Indicators |
|---|---|---|
| 1. Ethics and Responsibility | Performs clinical practice ethically and legally and serves the commu nity with dedication. | Makes appropriate medical decisions based on ethical and legal standards. Carries out clinical practice faithfully in accordance with the physician's role. Understands and implements strategies for preventing and responding to patient safety incidents. Serves the community through volunteer activities. |
| 2. Self-development | Manages and develops oneself effectively, builds a clear sense of prof essional identity, and fulfills the role as a member of the healthcare team. | Effectively manages and develops oneself. Explores various career paths and establishes a professional identity. Effectively fulfills roles as a member or leader of the healthcare team. |
| 3. System Understanding | Contributes to improving the healthcare delivery system. | Contributes to the enhancement of the health are delivery system. |
Medical Competency – Medical Knowledge
| Sub-competency | Description | Behavioral Indicators |
|---|---|---|
| 1. Mechanisms of Health and Disease | Ability to explain the mechanisms underlying medical problems. | Explains the normal structure and function of the human body. Understands the pathophysiology of diseases and applies it to diagnosis and treatment. Describes the symptoms and progression of common diseases. |
| 2. Diagnostic Investigation | Ability to appropriately select and interpret diagnostic tests based on clinical presentations to identify and reason through clinical problems. | Selects appropriate diagnostic methods necessary for diagnosis and treatment. |
| 3. Therapeutic Approach | Ability to appropriately select, apply, and evaluate treatment methods in clinical situations. | Selects and applies evidence-based medical/surgical treatments for major clinical situations. Selects and applies appropriate medications for different diseases. |
Medical Competency – Patient Care / Skills
| Sub-competency | Description | Behavioral Indicators |
|---|---|---|
| 1. History Taking and Problem Recognition | Ability to take a patient history focused on clinical situations and identify relevant problems. | Explains techniques for history taking in detail. Takes history based on the clinical presentation to identify risk factors and health problems. |
| 2. Physical Examination | Ability to perform appropriate physical examinations according to the symptoms and collect relevant information. | Performs basic physical examinations, mental status examinations, and functional assessments. |
| 3. Clinical Reasoning, Testing, and Treatment | Ability to reason clinically based on collected information and scientific evidence, and provide initial treatment. | Plans differential diagnosis and establishes appropriate treatment plans. |
| 4. Patient Education | Ability to effectively educate patients on disease management and preventive measures. | Explains basic disease management and preventive strategies. |
| 5. Procedural Skills | Ability to perform basic clinical procedures. | Performs basic clinical procedures appropriately. |
Scholarly Attitude
| Sub-competency | Description | Behavioral Indicators |
|---|---|---|
| 1. Lifelong Learner | Ability to continuously acquire knowledge necessary for medical practice throughout one’s professional life. | Gathers and critically evaluates medical evidence in clinical situations and applies it accordingly. Identifies personal learning objectives appropriate to one’s competency level and engages in lifelong learning. Reflects on learning outcomes to recognize strengths and weaknesses and implements improvements. |
| 2. Researcher | Cultivates the qualities required to conduct me dical research. |
Able to document medical concepts accurately. Analyzes and interprets results from medical research. Acquires various medical research methodologies and plans research in accordance with research ethics. |
| 3. Educator | Ability to teach medical knowledge and skills. | Educates patients and teaches medical knowledge and skills to peers. |
| 4. Community Health Advocate | Identifies and addresses health issues in the community. | Understands healthcare policies and systems to advocate for community health. Proposes solutions to community health problems in response to future changes in healthcare. |
6. Innovation and Future Adaptation
Technology Integration
- AI-Based Medical Imaging Analysis: Preparing for future healthcare technology
- Digital Health Literacy: Electronic medical records and elemedicine preparation
- Simulation-Based Learning: Advanced clinical skills training
Responsive Curriculum Development
- Environmental Health: Climate change and health implications
- Precision Medicine: Personalized healthcare approaches
- Global Health Security: Pandemic preparedness and response
- Healthcare Policy: Understanding healthcare systems and policy development
7. Supporting Infrastructure
Faculty Development
- Teaching Excellence: Regular faculty training in medical education
- Mentorship Programs: Structured guidance for student development
- Research Collaboration: Faculty-student research partnerships
Learning Resources
- Simulation Centers: State-of-the-art clinical skills training facilities
- Digital Learning Platforms: Comprehensive online learning support
- Clinical Training Sites: University hospitals and community healthcare partnerships
- International Partnerships: Global learning opportunities
8. Conclusion
The SyMBIOSIS curriculum at Pusan National University College of Medicine represents a comprehensive and innovative approach to medical education, preparing graduates for the complexities of modern healthcare. Through the systematic integration of basic sciences, clinical medicine, and medical humanities, combined with early clinical exposure and evidence-based learning, our students develop into competent, compassionate, and globally minded physicians.
Our commitment to continuous improvement, student-centered learning, and adaptation to future healthcare needs ensures that our graduates are well-prepared to serve their communities and contribute to the advancement of medical science and practice.